In this episode, we interview national nutrition expert Rebecca Scritchfield and get her thoughts on the Body Mass Index (BMI) measure and what it means for our health. Rebecca is a registered dietitian nutritionist, certified exercise physiologist, author of the book Body Kindness, and host of the Body Kindness podcast. Through her weight-inclusive counseling practice, she helps people make peace with food, find the joy in exercise, and create a better life with workable goals that fit individual interests.
- Rebecca’s thoughts on the validity of BMI. Is it BS?
- The relationship between BMI, health, and disease
- Can you be at a high BMI and still be healthy? How about vice-versa?
- Cultural factors that change how BMI should be interpreted
- Rebecca’s thoughts on weight stigma, and what to do when your doctor comments on your weight and recommends weight loss
- How to take care of ourselves without focusing on BMI
- & MORE
Resources:
- Rebecca’s website
- PSA: Healthy Eating Should Include Mental And Social Health, Too
- Body Kindness – Rebecca’s first podcast episode with us
- Regan Chastain’s “What to say at the doctor’s office” Printable cards
- Fearing the Black Body: The Racial Origins of Fat Phobia
SHOUTOUT TO OUR PODCAST SPONSORS:
Tired of wearing uncomfortable bras? Take Thirdlove’s online quiz to find a bra with the perfect fit and a premium feel, among more than 70 sizes – including their signature half-cup sizes! Go to ThirdLove.com/FOODHEAVEN and get 15% off your first purchase!
How to subscribe:
- iTunes (apple)
- Google Play (android)
- SoundCloud (both)
Connect with us online:
- Instagram @foodheaven
- Twitter @foodheavenshow
- Facebook @foodheavenmadeeasy
- Pinterest @foodheavenmadeeasy
Our podcast is released every Wednesday. In each episode, we cover tips and tricks for making lifelong sustainable healthy living changes to upgrade your diet and health. We also interview leading experts in the field of health and nutrition to pick their brains on how to cultivate a healthy life that you love. We hope you enjoyed this episode, and we’ll catch you next time!
EPISODE TRANSCRIPT
Speaker 1: The following podcast is a Dear Media production.
Wendy Lopez: Shopping for bras has usually been a headache for me up until I started using ThirdLove. I used to feel like I had compression bands around my chest, yes, compression bands, where like there was wiring poking me. It just never seemed to work out. And honestly, most times, I just opted for a sports bra, or all my friends know, I just wouldn’t wear a bra, TMI, because I just wanted to avoid the mess. Ladies, as you all know, having the right bra is so, so important. Go to thirdlove.com/foodheaven for 15% off today.
Wendy Lopez: All right, let’s get into our episode.
Wendy Lopez: Hey, it’s Wendy.
Jessica Jones: And it’s Jess. And you’re listening to the Food Heaven podcast.
Wendy Lopez: Your online resource for delicious and nutritious living.
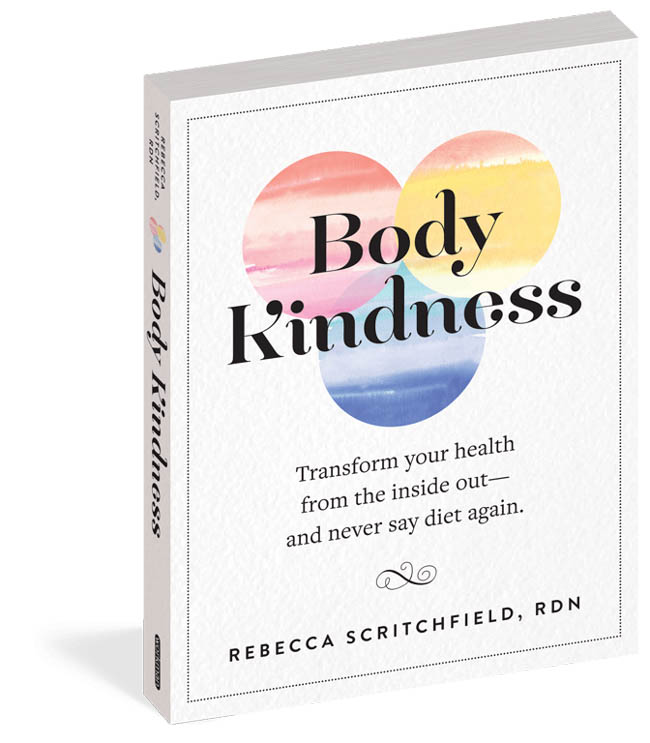
Wendy Lopez: Hey everyone, thank you so much for tuning into the Food Heaven podcast. Today, we’re talking with Rebecca Scritchfield, registered dietitian, certified exercise physiologist and author of the Body Kindness book, and a host of the Body Kindness podcast. Through her weight inclusive counseling practice, Rebecca helps people make peace with food and find the joy in exercise. Rebecca has influenced millions through her writing, podcast and appearances in outlets like NBC, CNN, The Today Show, Washington Post, and more.
Jessica Jones: Today we are going to be talking with Rebecca about BMI, which is body mass index. And we’re going to pick her brain on whether or not BMI is BS. We actually had Rebecca on the podcast a couple of years ago talking about Health at Every Size and Intuitive Eating and her whole practice of Body Kindness and taking care of yourself from the inside out without dieting. So if you want more about her background and how she got into this work, make sure to check out the Body Kindness episode.
Jessica Jones: But today, we’re just going to jump right in and really get an understanding on what the research says when it comes to BMI and is it something that you guys should use as a determining factor of your health. So, welcome to the podcast, Rebecca.
Rebecca Scritch: Thanks for having me back.
Jessica Jones: Yay. So excited to have you. So we just want to jump right in. And I know that there may be people who want to learn more about you and your background, but we’re going to refer you guys to the initial episode we did with Rebecca, where we talked all about how she got into nutrition and how she transitioned into Health at Every Size. But today, we’re just going to jump right into BMI. So just tell us, first and foremost, in a nutshell, is BMI BS?
Wendy Lopez: And what is BMI? Because I think-
Jessica Jones: And what is BMI?
Wendy Lopez: Yeah. There might people that are like, “What the hell is a BMI?”
Jessica Jones: Good point.
Rebecca Scritchfield: I was like, “I want to say the answer. Yes, I hate it. Go away. Never come back.” But yeah, I just I’m 100% aligned with you that I’m always talking to my clients about it, even friends. And if you really think about it, if we just reflect in our world, you can’t see the doctor, your kids can’t go to the school nurse, you can’t do a Google search about a health topic or read a book or listen to a podcast that’s about health without hearing about BMI, which stands for body mass index, but that’s how pervasive it is.
Rebecca Scritchfield: And I think that’s an important note to make, is that it is literally everywhere. And so the idea that it’s so prevalent makes you think that, “Well, this must be true. This must be important. I must do something about it.” And so it ends up coming along with a lot of fear because it’s tied to fear of, “I’m doomed to poor health if my BMI isn’t the perfect number.” So I just want to empathize with the listeners for a minute that you can’t go anywhere without hearing about it. And there’s so much confusion around it.
Rebecca Scritchfield: So to back up to help people understand it a little bit better, I think it’s important to just take a look back at the history of it. And the bottom line is to understand that it is a really old equation. It was created in the 1830s. And think about this, it’s a time when we had no computers, not even like a little calculator. And we certainly didn’t understand the complexities of weight and health at the time. So a mathematician designed it to just try to give a very rough idea of someone’s weight status by dividing their weight by their height.
Rebecca Scritchfield: And so it was old, but then as time went on, I think it was around the late 1950s, it was adopted by a life insurance company as a way to look at weight in terms of health. Now, think of a life insurance company, they’re a business that is there to make money, and so they want to exclude people from life insurance policies because, “Oh, well, maybe you did this to yourself with this early death.” So it starts to get really twisted. A life insurance company is a business that’s not your doctor, so why is your doctor talking about BMI?
Jessica Jones: Yes. So true. When you really think about the history and like wasn’t something that was really studied and has a lot of validity to it, it sounds like, yeah, it hasn’t really been studied and it was put out there by a business machine to make more money. So, that’s a really good point.
Rebecca Scritchfield: Well, and another good point about it that I always like to let people know is that, what is the attachment to it in medicine and public health. And this is the bottom line with that, it’s very easy to obtain information because you just need two factors, height and weight. You don’t even need a tape measure. So when you think about it in the context of looking at populations, something that could be used worldwide, it is a really easy to obtain, quick, easy piece of information. But what we need to remember is that there really is no evidence that the information it obtained is meaningful, that it actually predicts useful information about health or disease risks.
Rebecca Scritchfield: And what’s really scary is that in our culture today, it can be used to determine how much our health insurance policy is going to cost, whether or not they want to include you or exclude you. And it can even be used to determine whether or not they’re willing to give you necessary medical care such as surgery, whether that might be for knee or hip, or even something like in vitro fertilization, which folks argue that it’s a form of eugenics. If you can use somebody’s body mass index to say, “Nope, we’re not going to do IVF for you,” you’re basically taken away somebody’s chance to have a baby because of their BMI, but you would help a lower weight person.
Rebecca Scritchfield: You’re not giving them the opportunity to allow… first of all, the joy of becoming a parent, but then also moving their genetics forward. So it’s really political too.
Jessica Jones: Yeah. And it’s also crazy how many assumptions are made off of someone’s BMI because a lot of providers are literally just plugging in the numbers and they’re like, “This is what you need to do because this is your BMI.” And there are no questions asked whatsoever about medical history, family history, habits at all. There’s this assumption, I think, among medical practitioners, but also just among people who are familiar with BMI, that people that have lower BMI are automatically deemed healthy, people that have higher BMI are not healthy.
Jessica Jones: So I was wondering if you could share some of your insights around that and maybe even like any research that you’ve come across that’s really interesting that discredits that whole idea.
Rebecca Scritchfield: Yeah, sure. So whenever we’re talking about assumptions, what we’re really talking about is our weight bias. That’s a cultural construct for us, it was before since any of us were born. But there was a time when higher weight was powerful and desirable and it’s just now in our lifetime it’s, thin has all the power and higher weight, you’re going to be more oppressed. And so as human beings, we’re often just trying to rate our opinions about people. Partially, it’s how humans think, our brains need to put it in that context of, “Is this a good thing or is this a bad thing?” But then on top of culturally what we say we value, then there are winners and losers.
Rebecca Scritchfield: I also want to help people understand that, that there’s no personal blame where it’s just like, “What can I do to lower my BMI?” Or, “I’d like to lose weight.” A big part of that has to do with the fact of that you would experience less bias because of how our whole society works. With respect to, well, how could that judgment mischaracterize people? There’s a lot of interesting things. One really big study that was published in The Journal of American Medical Association ran the statistics and actually showed that people who had a BMI that was overweight or obesity grade one actually had the longest chances for longevity.
Rebecca Scritchfield: And it was people who had a BMI that was considered “normal or underweight,” who had a reduced life expectancy. It was pretty mind blowing because the way the statistic worked out, it didn’t really match what we would think based on our social judgments. And then again, well, people would say, “Oh, so we’re just supposed to eat donuts and never exercise?” Don’t jump to those conclusions. No, it just continues to contribute to the flaw that that number is really not saying, “Well, if you fit this category, you must be doing something wrong.”
Rebecca Scritchfield: One gigantic reason for the flaw is that it does not take into account muscle mass or things like where there might be diversity in bone density and everything like that. Because the other thing about how these numbers were normalized, is it was based off of white males as opposed to… There wasn’t exactly a diverse population that was used to validate this equation either.
Jessica Jones: That’s so powerful because I feel like, especially as people of color, we’re always… Like a lot of times, we might have a higher BMI. So many of my patients are black women, and they automatically feel like, “Oh my God, there’s something wrong. What do I need to do? Do I need to lose weight?” And so basically what you’re saying is that even with this tool that isn’t necessarily that accurate to begin with, it also doesn’t even apply to anyone who isn’t a white male. So, at best, would you say it’s irrelevant for people of color? How would you say people of color should navigate BMI?
Rebecca Scritchfield: Yeah. Well, I think that it’s… I can point to a couple studies that are worth taking a look at. I’ll give this the bottom line sum and then I could give you the links for the studies if you’d like to share them in the show notes. But one was in 2011 and it was published in the research journal Obesity. And what they found was that white women with BMI of 30 or more and a waist circumference of 36 inches or more were at a greater risk for diabetes, high blood pressure and high cholesterol, but black women who had those same numbers were considered medically healthy.
Rebecca Scritchfield: So part of what this study is showing is that there can be an association with certain BMI factors that could increase your risk. It doesn’t mean that you’re going to get certain conditions because there’s so many factors, genetics being one of them. And lifestyle does play a role, but not as an important role as we think. But then when you segment it out between white women and black women, the black women were not at a higher risk, so there was a difference in how they experienced the risk. But that’s not common knowledge. You’re not likely to go to your doctor and be like, “Well, you know… .”
Rebecca Scritchfield: And again, how you were mentioning assumptions. The way the whole system works is you show up for your medical appointment, before you even see the doctor, you step on a scale. And the reason why you do that is because it’s recommended. It’s a recommended screening by something called the US Preventative Taskforce. And it has a B grade, which it’s not even… It’s just kind of like, “Eh, we think this could be helpful, but it’s a recommended screening that you weigh the client, calculate their BMI, and then you talk to them about an intensive behavioral program if their BMI is of a certain number, so the higher BMI.”
Rebecca Scritchfield: What’s fascinating about that approach is that, number one, we are not educated that it’s an optional screening that we can decline. And in fact, I’ve talked to clients about this and talked about refusing to being weighed at the doctor’s because it was a traumatic experience. And sometimes they’ll get pressured like, I might need to know this number, and why don’t you want to get weighed? You can literally say, “Unless it’s medically necessary, I decline to have this screening.” But the other thing that it does in the process is, it might flag them to give you counseling that you don’t really need, because you’re in there for an earache and you’re happy with your habits.
Rebecca Scritchfield: But instead of them talking to you about your habits, they say, “Oh well your BMI… ” and blah blah blah and doom and gloom, that’s really unhelpful. It actually can create a lot of shame and healthcare stress, which could lead to future healthcare avoidance. But the other element is, this is back in the insurance company thing is, when they have that conversation with you, they check a box and they get to bill insurance for it. So I don’t want to think that doctors are malicious, all doctors are malicious, I want to think that they genuinely care about helping people. But now if you see how twisted all of this stuff is, it’s recommended that you do this, so we don’t know it’s an optional screening, and your doctor’s going to bring it up.
Rebecca Scritchfield: And if it’s something that is important in how you have those conversations about your self-care and your wellbeing, that they’ll bring it up because they were to, and they’re going to get paid by insurance to do it. So it’s this whole system that keeps BMI in medicine and then yet we have these research studies that show that it’s really not that helpful. One other study that looked at black people, it showed that black people had less body fat than white people. So even when they had the same BMI and waist measurements, that they had lower body fat.
Rebecca Scritchfield: And so there’s this belief that black people might have more muscle mass, and so that is really going to mess up their BMI calculation. So at any rate, the fact that we walk around so afraid of what our body mass index is, or that depending on where we land, that that means something about our health, that is what’s problematic and that we need to reframe our relationship with our weight or BMI and even how we see our health and wellbeing.
Wendy Lopez: Yeah. When I’ve spoken to healthcare providers about this topic, what usually comes up is that, “Well, what about the research, and the research?” There’s so much research out there about BMI and about how it’s correlated with all of these chronic conditions. And usually all of the factors that we’ve spoken about, like medical history, family history, genetics, lifestyle factors, all of these things are usually never discussed, and there’s such a focus on BMI. So how have you navigated talking with healthcare providers that are BMI focused? Because it’s really tricky.
Wendy Lopez: I’ve had these conversations and clinics that I’ve worked at and it’s like there’s just always this focus on, “Okay, but what about all of the research that has been done for all of the years?” What do you have to say to that?
Rebecca Scritchfield: Sure. So generally speaking, I might get into a conversation just about the bias of research in and of itself. Even research is rooted in bias about weight and white supremacy, what gets funded, who gets chosen to study, how long is the research study? So, especially when you’re looking at things like weight and BMI, most studies are less than a year. Some are even like, oh, in a 12 week program with 11 people. So very small study size and all these other things. But unless you’re looking at people in two to five years later after an intervention, then you’re really not capturing what could be a wait cycle, meaning that you employed significant lifestyle changes with the hopes that that person would lose weight and improve their BMI number.
Rebecca Scritchfield: And then what ends up happening is we, because we have a set point range, even if we maintain those habits, and we might even have better lab value markers, but even if we maintain those habits, some people will cycle down and wait, and then back up again. And we saw that in the Look AHEAD Study, which it was ended a few years early due to futility because they found that even with intensive lifestyle, that people with diabetes still had a higher risk of cardiovascular events. So, it doesn’t mean that we don’t work to improve people’s quality of life, it’s just that looking at research and assuming that, “Oh, all research is a gold standard and if one study said it, it must be true.”
Rebecca Scritchfield: Knowing the way that research works, it’s like, “We have a guess, and we think we might be right, and we’re going to get a little bit smarter in this one study. And then that’s going to lead to another study because we learned one little new thing.” It’s a cycle. Research always begets more research. And yes, we need it and we will learn and grow, but using the research to be a definitive thing as, “And this is why I need to take this study and apply it to this individual,” I actually think it’s really unhelpful. And I’ll give you a specific example for that too. In a conversation with another helping professional, I often, I want to meet them where they’re at, and I want to start with empathy and more questions, seeking and peak curiosity.
Rebecca Scritchfield: So I might ask the question like, “Well, how would it be helpful to start with things like BMI and weight first?” As you’re flagging factors that would lead to the next conversation about self-care and wellbeing and healthy lifestyle. And I want to get their answer and it might point to research. But what is fascinating is that if you start with the BMI, you actually might miss a screening opportunity for people with heart disease and type two diabetes risks because… There was a really large study, there was more than 40,000 people in it. This was published in the International Journal of Obesity too that suggested that nearly half of the people who are categorized as overweight were cardio metabolically healthy, while 30% of the people within the normal BMI were not in good shape.
Rebecca Scritchfield: So if you start with the BMI and, “Oh, it’s normal, I’m not going to have that conversation,” what if they actually need a conversation about self-care? You’re missing them. And then you’re targeting the people who have the higher BMI, and what if everything’s hunky Dory there? And I’m oversimplifying it, but I think that the end result is questioning how helpful is it to start with BMI and weight to guide the next conversation?
Jessica Jones: Yeah. I love how you focus also on empathy because I know at the end of the day like we’re all trying to help people, for the most part, and we want people to be healthier and we’re coming from a good place. So I’d like just coming from that place of curiosity, I think can make people feel less defensive in just presenting like the study that you just mentioned. I’ve seen that study as well, and I’ll use that in some of the talks that I do just to illustrate that, “Yeah, it doesn’t always necessarily correlate the way that you think it would in terms of people who are at higher weights being unhealthy.”
Jessica Jones: One question I have as a followup is, so then what are the things… Can you talk about the things that you would look at as opposed to BMI? So let’s say BMI is BS. How do I know if I am metabolically healthy?
Rebecca Scritchfield: Sure. So knowing family history, I think is really important because most chronic diseases are genetically heritable, around 80%. And weight is also genetically heritable around 70 to 80%. So I would want to know about family history, I would want to know about their concerns about their health and wellbeing. So there are things in people’s lives that they can’t easily control, which could be how much money they’re able to make them their job, which plays into the resources they have for food and movement, or their responsibilities that they might have, whether they’re a single parent or just two busy, really working parents that have childcare responsibilities as well as job responsibilities that also impede on their resources for things like time and money.
Rebecca Scritchfield: So really I think it’s about working… Every individual is different and they have a different lived experience, they’ve a different genetic history, different amount of resources, a different set of interests. I think that because their culture is so weight centered, and I’ve kind of resolved, I’m always going to get clients who come and sit down and say, “Hey, I got to do something about my weight,” even if what they really mean is they want to make improvements to their habits or they do have a weight concern, because again, they like to conform a little bit better.
Rebecca Scritchfield: It’s not about that question ever going away, it’s about how do you listen with empathy and really provide good support of help and remember that the people we work with, like we’re really emotional-driven kind of feeling creatures, we want to take good care of ourselves. I think naturally we want to feel good, so we do want to get better sleep, but that might be challenging, so how do you help someone get better sleep? We might understand it’s important to not smoke and not drink too much, but we might need help with quit programs or ways of managing our stress and engaging in warm, mindful breathing and meditation to help us move further along in that category.
Rebecca Scritchfield: And absolutely, we might have an interest in healthier eating patterns, but we need to find something workable based on totally how to do etc, etc. But I think so often what’s presented to the people we work with is this eurocentric, like thin young white woman standard of like, it’s got to be a green juice and Lulu lemon yoga pants and SoulCycle. And it’s like, “Look, I’ve been to SoulCycle and I do like green juices, you know.”
Wendy Lopez: Oh my God, I love SoulCycle.
Jessica Jones: I know.
Rebecca Scritchfield: You know what I’m saying?
Wendy Lopez: I love a green smoothie.
Rebecca Scritchfield: So you get it, right?
Wendy Lopez: We get it.
Jessica Jones: Yeah, we totally get it.
Wendy Lopez: Having the right bra can really help boost your confidence and self esteem. You all know about my experience with bra shopping. So one ThirdLove reached out. I was a little hesitant, I’m like, “Okay, is my chest going to feel suffocated with these bras?” The verdict, absolutely not. ThirdLove offers over 70 sizes and even include half cup sizes. They have a Fit Finder tool online, which you can try at home. You don’t have to have stranger awkwardly wrap a measuring tape around your boots. While other brands charge more based on sizing, which is really messed up by the way.
Wendy Lopez: ThirdLove bras cost the same no matter what the size. They’re really big on inclusive sizing, and what I loved about their site was that the bra models they use are all shades and sizes, it’s not the usual size to model. They also have a 100% fit guarantee. Every customer has 60 days to wear the bras, wash it, put it to the test, and if you don’t love it, return it. And ThirdLove will wash it and donate, it to a woman in need. Yes, ThirdLove is amazing. And this is hands down the most comfortable bra you’ll own. No weird rashes, itching or marks on your back. ThirdLove knows there’s a perfect bra for everyone.
Wendy Lopez: Go to thirdlove.com/foodheaven right now to find your perfect fitting bra and get 15% off your first purchase. That’s thirdlove.com/foodheaven. All right, let’s get back to our episode.
Jessica Jones: Okay. One thing we haven’t talked about is weight stigma. Can you just talk about what that is and how that fits into all of this conversation?
Rebecca Scritchfield: Yeah. I think that first and saying it, I want to just talk for a second about our common humanity and that we’re all products of our culture. Our culture creates who we are and how we think and what we do. And from the time of one years old, anything that we absorbed in the world, we started to kind of make it like a copy of it in our mind and an imprint. So any character that we ever had access to, play dates, what was on TV, anything at all, things that were said, it all impacts us because of the voice of who we are and everything.
Rebecca Scritchfield: So the idea of, well, how does that relate to… Well, what do we believe about bodies? And we end up creating these belief systems that there are good bodies and there are bad bodies and the good bodies are thinner and the bad bodies are fatter. And we actually see it play out and how it can impact somebody’s quality of life. Rebecca Puhl is a researcher on weight stigma and she has shown that as your BMI climbs, you have less, fewer job opportunities and you’re less likely to get promoted. So that hits people right in their pocketbook. And it can really be really unintentional microaggression stuff that happens.
Rebecca Scritchfield: If you’re working out at a gym and you see someone who’s at a higher weight and they’re sweating, that urge you might feel to like offer a congratulations for them or that urge you might feel, you’ll be like, “Yeah, nice try, good for you.” But you wouldn’t do that to the other thin person on the other treadmill next to you because you might automatically believe that they’re a beginner. The truth is, you don’t know if they’re a certified personal trainer just pushing themselves. And so it happens all the time down to like what size clothing, is it comfortable workout clothing is available to people at higher weights?
Rebecca Scritchfield: And if you’re a higher weight and a vegetarian, you must be doing that because you hate yourself and you’re trying to lose weight. And that’s not necessarily true, and so it’s things like that that impact our beliefs that then might impact how we treat somebody out. That’s what we want to do, we want to challenge our own biases. This is everyone, not just health [inaudible 00:27:44] everyone. If we started from the beliefs that all bodies are good and that there are ways that the culture may have told me that certain bodies are good or bad or how to make assumptions, even if my intent is to be a helpful, caring person, that intent doesn’t really lead to impact.
Rebecca Scritchfield: And so if we could just start saying that we don’t know anybody’s individual story and we don’t want to make assumptions about them. We’re actually really doing magnificent work to fight weight stigma just by challenging our own bigotry because that reduces the oppression that they might feel. But weight stigmas is much more about the systems and structures that are in place that make it hard. And so like the example I mentioned earlier where you walk in the doctor’s and you weigh and you have that conversation based off BMI to if you walk into a store you’re super privileged. You might not like what you see in the store, but you’ll find stuff in your size.
Rebecca Scritchfield: And there are people who are at higher weights, I think it’s 67% of American women are a size 14 or higher and they’re getting better in fashion, like for cheap clothes, for higher weight people. But the fact that it’s such a larger percentage of people and clothing options go down as your size. So you have to want to challenge why that is and what we all need to know about it is because we don’t have to make those daily stressful decisions. Like, “Am I safe or am I in danger? or am I safe with the doctors? Am I safe on the airplane? Is somebody going to yell at me for buying marshmallows at the grocery store today?”
Rebecca Scritchfield: That daily chronic stress builds up and actually shows up in the body as risk factors for inflammation and diseases. And so it’s not that they’re not trying to get joyful movement in or not that they’re not trying to make an effort to eat better, it’s just people won’t leave him alone with the assumptions. The more privileged people from the healthcare standpoint and just for people who have sized privilege to just try to learn and grow in this area, try to reduce the assumptions that you make, try to send love, kindness and compassion to others and you will be doing your part to make the world better. But ultimately, we got to kind of shut it down and do it all over again.
Wendy Lopez: Yeah, shut it down. I’m with that. I’m just like, all this weight stigma especially, it’s everywhere but especially in health care, people don’t want to go to the doctor because they’re like, “Oh my God, I’m going to hear the same shit over and over again.” And one of my friends, she literally forwarded me, last week she forwarded me this email from her doctor because she needed some kind of prescription and she’s like, “Well, since your BMI is this, you’re at high risk for like liver disease, kidney disease.” It was like she was going to die. And she’s like, “Therefore, this is my recommendation. You need to get tested.”
Wendy Lopez: And she was devastated and like she loved going to this doctor. And she was like, “I don’t think I want to go again.” And I hear this all the time from my friends, especially my friends who are of size, they’re like, “I don’t want to see my doctor again because once that conversation came up about BMI, I completely shut down and I felt like they were judging me. They didn’t ask me any questions about my life.” And I know that this is something that a lot of people struggle with when going to the doctor and they’re like, “Shit, I’m just not going to go.” How do people navigate that? When they go to their appointments and doctors are constantly bringing it up because it can be really scary to speak up and say, “Hey, I don’t appreciate that. That makes me feel really uncomfortable.” Have you found any useful ways to talk with your provider about that?
Rebecca Scritchfield: Yeah, 100%. First of all, keep doing what you’re doing and validating for everyone you work with that you are not the problem, the system and the structure and the doctor is the problem because they need to hear that from you a million times before they’ll believe it. And I mentioned it briefly, but just to reinforce for you, and I’ll share this research study too because it was one of my favorite studies that came out in 2018 that actually showed a model of what leads to health care avoidance, and as a persons body mass index climbs, they have higher experiences of body related guilt and shame related to the healthcare encounter. But it’s when the guilt and shame lead to healthcare stress, that’s the mitigating variable. When they have stress over the healthcare encounter, they are likely to avoid going back.
Rebecca Scritchfield: And so if we think about healthcare avoidance, that should be our concern about health and not the obesity epidemic. Like what are doctors doing wrong that are making it so that people avoid going to see the doctor. Then if you think about, “Oh, well, how are we, people cost this much more money on the health care system? They quote burden, you’ll even read about… Well, could things be caught sooner with less expensive tests if they weren’t experiencing weight stigma in the medical practice.
Rebecca Scritchfield: And there have been studies, one woman, she dedicated her obituary to talking about all the weight stigma that she experienced through her entire life, that went viral. That was a big story that went viral. Somebody whose cancer got missed for a couple of years because the answer was always, “Lose weight.” She was like, “Nope, I’m really out of breath.” Ended up being lung cancer. This is a real problem in the profession. And so back to, well, how do we empower our clients? You set big boundaries, assuming you have the privilege to have health insurance, assuming that you have the privilege to choose the doctors.
Rebecca Scritchfield: Literally, from the get-go and write it down in a note or in a letter, “This is how I need you to respect my weight and my body. I’m going to refuse all weights unless it’s medically necessary. These are things you can ask me about. You can ask me about joyful movement, you can ask me about sleep, you can ask me if I need help with my food ideas or eating patterns.” You can literally set the guides for how you want them to be able to treat you. Many doctors are not trauma informed and so how might you explain whether it’s the trauma of chronic dieting or maybe you had an eating disorder, maybe you had food insecurity as a kid and that you have worked your way through that in therapy, but it sort of has adjusted your relationship to food and body and even talking about food and your weight is re-traumatizing.
Rebecca Scritchfield: We hope that the doctors will become more educated so they do less harm, but while we know that there’s harm being done in the medical profession, the number one thing we need to do is figure out the boundaries and tell people how we want to be treated and demand that of them. There are some simple tools, I’ll give you the link to Ragen Chastain. She’s a fat activist and has a blog called Dances With Fat. She also happens to have the Guinness World Record for the highest weight female who’s completed a marathon.
Rebecca Scritchield: Again, back into that, don’t judge people by their size, but she has these awesome cards that you can pronounce and it’s literally like, “This is how I want you to take care of my medical needs.” So that could be helpful to people too.
Wendy Lopez: Thank you so much for those resources. I’m like writing everything down because I have patients where I literally have to coach them through the trauma of seeing a doctor or seeing a specialist. And sometimes it’s like a whole visit of like, “Okay, what are you going to say?” Like how to try to make things like less triggering because people… You’re so right, we don’t know someone’s history and someone’s trauma and someone’s potential eating disorder, disorder eating, their habits. And a lot of these folks are like super active people who just happened to be at higher weights and the doctors make so many assumptions and don’t give them the care that they need. And it just makes me really upset.
Wendy Lopez: And I feel like sometimes doctors, and I know everybody means well, or healthcare providers in general, will just label people, “Oh, they’re non-compliant.” It’s like, “Okay, I hate that.”
Rebecca Scritchfield: Yeah. It was like that sound of the nails on the chalkboard, that’s someone on my ears when I heard non-compliant. Because that is, every time I hear that, I always start with the word gently, if you ever see me on social media, going, “Gently… ” and then blah, blah, blah to somebody who used the word non-compliant because that’s when I get back to the empathy part, the lived experience. So somebody isn’t able bodied or they are going through a dialysis clinic or they have a new diagnosis of diabetes. There is so much shame people carry with them about having any kind of health problem.
Rebecca Scritchfield: And that is a problem in and of itself and it’s rooted in this belief that we have 100% control over our health our entire lives and if we happen to get anything ever, we caused it and that we are now responsible for getting ourselves out of it. So when you mentioned people who are doing reasonable healthy habits but they’re still going to be judged, even if your lived experience has been that, “Oh yeah, I think I could’ve done better here, here,” just the idea that you need medical care is now the source of shame and blame, you’re not doing that to yourself. That shame cycle is a result of what our culture says you should be doing, and that’s just so messed up.
Rebecca Scritchfield: The word is health care. Doctors go into medicine to do no harm, don’t we? Like you said earlier, our intention is to help people. And so it’s like having this really high compassion, not judging about non-compliance. There is a million reasons why somebody might have difficulty doing the things that are on the list, that we want them to do, that they wish that they could do. And it could absolutely have to do with practical things like resources, it could do with mental health. And frankly, we’re not even talking about health, we’re talking about mental health too.
Rebecca Scritchfield: That’s a whole other barrier that we need to be able to consider from the folks of us that are like, “Hey, let’s add a fruits and veggies to our shopping list this week.” We also need to be trained and understand what it’s like to struggle with mental health and how that might impact our self-care abilities.
Jessica Jones: Yeah. I just wrote this article for Self about how healthy eating is about your mental and social health too because that’s often overlooked. But that’s actually a good segue because we talk so much about BMI and how it can be problematic. And I just want to spend a second to talk about how people can take care of themselves. What are your recommendations without focusing on BMI?
Rebecca Scritchfield: Sure. Well, I think one of, if there was the first step for everyone. I think you take your hands and you place them over your heart and you soften your eyes and as you breathe you repeat to yourself, “It’s okay, I am good. I can handle this, I will take care of myself.” And it’s a form of affirmation that is connecting. We do all have an inner caregiver in our minds, there are voices there, but it’s very quiet, because of the diet culture and all the other messages. We got the perfectionist, the judger, the toddler who just wants to do whatever, the rebel who is like, “You can’t control me.” And we have this caregiver voice.
Rebecca Scritchfield: And I honestly think that if we start with this “it’s okay” a simple form of self compassion because a lot of people are like, “Take a bubble bath and reduce your stress.” You jump kind of too far because a lot of people have really challenging problems that no amount of bubble baths are really going to solve. So it’s this idea that nobody gets a pain-free life and yes, I might be going through something really difficult and you feel uncertain, you’re hoping confidence is pretty darn low, and what helps you shift to a little bit more optimism and a little bit more hope that things can get better, like, “I can create a better life for myself,” it starts with that compassion that, “It’s okay, this is hard, but I can handle this and I’m going to take care of myself.”
Rebecca Scritchfield: And then all the other further steps, it’s in line with your caregiver, what would my caregiver do? And what everybody needs to do is going to look a little bit different, but I would highly recommend that you stop creating a giant list of everything that’s wrong with you and everything you need to fix, that’s like letting your inner critic run roughshod. You’re going to finish that listing, like you suck and you’re not going to do anything. Start with that compassion practice and just start picking a couple of things. One or two things that you’re going to pay more attention to, whether, “I’m going to drinking more water. Okay, I’m peeing clear again, and I do want to get a little bit more sleep.”
Rebecca Scritchfield: And then, “All right, let me cook a couple more meals at home than I typically would.” But a lot of times these people think that it’s, “That’s not enough.” And it’s actually a gentle pattern that creates the sense of achievement that makes you feel even more confident that you could build from there.
Wendy Lopez: Rebecca, have you thought about doing some kind of guided meditation audio book?
Jessica Jones: I know. Or was I doing a meditation as you were saying it.
Wendy Lopez: As you were saying it, Jess over here was like holding her heart. That was a really great activity. I love it. That was good.
Rebecca Scritchfield: Maybe one day.
Wendy Lopez: Yeah, that’s, that’s really helpful I think for people to just pause, take a few seconds, practice gratitude, and really just align themselves with the here and now. I think that’s a really great activity to do, to just check in with yourself. This has been great. We love having you on, as always. Please tell everyone where they can find you.
Rebecca Scritchfield: Yeah, check out bodykindnessbook.com/start, and you can get a free e-course from that page. And if you’re a helping pro, you can let me know because I like to reach out to helping pros with other opportunities. And I’ll check in with you on how you’re doing with your Body Kindness practice.
Wendy Lopez: Awesome. Thank you so much Rebecca. We’ll catch you next time. Bye.
Rebecca Scritchfield: Thanks for having me.
Jessica Jones: Bye.
Wendy Lopez: Bye. Thank you so much for tuning into another episode of the Food Heaven podcast. If you like this episode, you already know the deal. Go to iTunes right now, leave us a review because this really, really helps us. I know you might think it’s like, “Oh, it’s not a big deal. I’ll get to it when I can.” No, it really helps us grow the podcast, so make sure you get on it right now. Listen to this listener review, “I’m always looking for perspective from young black women, so I really appreciate Wendy and Jessica’s work around health and nutrition. I find the podcast to be helpful, relevant, and fun to listen to. I’ve learned so much from these ladies and I will continue to tune in.”
Jessica Jones: Oh, thank you so much for that really sweet review. We really appreciate it and for those of you who don’t know, our podcast is released every Wednesday. And each episode, we cover tips and tricks for making life-long, sustainable, healthy living changes to upgrade your diet and health. We also interview leading experts in the field of health and nutrition to pick their brains on how you can cultivate a healthy life that you love. We hope you enjoyed this episode and we’ll catch you next time. Bye.
Wendy Lopez: Bye. Did you know that ThirdLove offers free returns whenever you need it? Well, I actually did need it. I wanted to adjust the sizing a little bit and the process was so easy. All I had to do was send the bras back using a prepaid label and I got my new bras within a week. They communicated with me every step of the way. And then at the back of my head, I’m like, “Okay, this is customer service to a whole another level.” To check out their amazing bras, go to thirdlove.com/foodheaven and get 15% off today.


Leave a Reply